Key points
- Chlamydia, a sexually transmitted disease, can also cause symptoms in the mouth and throat, known as oral chlamydia.
- Oral chlamydia is contracted through oral sex with an infected partner and may not always present noticeable symptoms.
- Diagnosis of oral chlamydia is typically done through a throat swab test, and it can be effectively treated with antibiotics.
- If left untreated, chlamydia can increase the risk for other serious health problems, including HIV/AIDS and infertility.
- To avoid oral chlamydia, the NIH recommends using a barrier method during oral sex, staying in a long-term monogamous relationship, and regular testing. Solv can assist in locating chlamydia testing providers in your area.

Chlamydia is a sexually transmitted disease (STD) caused by a bacteria called Chlamydia trachomatis. This STD usually affects the genitals, but can also cause symptoms in the mouth and throat.
The CDC advises that oral chlamydia be treated right away to reduce your risk for other infections, including other STDs. It is important to know about oral chlamydia symptoms, how it’s treated, and how you can find a high-quality treatment provider using Solv.
Is oral chlamydia a common thing?
Yes, it is possible to get oral chlamydia, which causes symptoms in the mouth and throat. In 2018, four million cases of chlamydia were reported in the United States, though the Centers for Disease Control and Prevention (CDC) estimates the number of infections may be much higher because many people do not experience noticeable symptoms.
The exact prevalence of oral chlamydia is unknown, as it is typically less common than genital chlamydia. However, it’s important to know that it can happen and that taking the necessary steps to avoid this STD may help reduce your risk for infection.
How do you get chlamydia in the mouth?
Also known as pharyngeal chlamydia, oral chlamydia can be caused by having oral sex with a partner who is infected with chlamydia.
According to the CDC, chlamydia in the throat and mouth is caused by giving oral sex to a partner who has an infected penis, vagina, urinary tract, or rectum. Oral chlamydia can also be caused by receiving oral sex on the penis, vagina, or anus from someone who has chlamydia in the throat.
What are chlamydia throat symptoms?
Many cases of oral chlamydia do not cause symptoms. However, according to the CDC, when oral chlamydia symptoms do occur, they may include:
- Sore throat (dryness and scratchiness in the throat)
- Mouth pain
- Mouth sores that don’t heal
- Cold sores (sores around the mouth and lips)
- Patches of redness with white spots
- Swollen tonsils
- Dental problems
- Chlamydia bumps on the tongue (in rare instances)
Some symptoms of oral chlamydia are the same as those associated with other types of health conditions. Visit your doctor to receive a proper diagnosis if you are experiencing any unusual oral symptoms, or if you think you have an STD in your mouth.
How is chlamydia diagnosed and treated?
Chlamydia can be diagnosed with a STD lab test. The NIH reports that males who want to be tested for chlamydia are asked to provide a urine sample, and females are given a long cotton swab they use to collect a sample from their vaginal areas. However, these diagnostic methods are usually only effective at diagnosing genital chlamydia — not oral chlamydia. Oral chlamydia can usually be diagnosed with a throat swab test in both males and females.
Oral and genital chlamydia can be effectively treated using antibiotics. Patients may be asked to refrain from engaging in any sexual activity for at least seven days until the infection has been cleared, according to the NIH. If you are diagnosed with chlamydia, your doctor may recommend taking all your antibiotic medication until the medication is gone, even if your symptoms have fully cleared.
What happens if chlamydia is left untreated for too long?
When left untreated, chlamydia can increase your risk for other serious health problems, including HIV/AIDs and infertility.
Chlamydia can weaken your immune system to make you more vulnerable to other infections and diseases, including other STDs. According to the NIH, n females, untreated chlamydia can cause pelvic inflammatory disease, ectopic pregnancy, and infertility. In males, it may lead to infertility and infection of the epididymis. Untreated chlamydia may also cause arthritis, reports the NIH.
How to help avoid oral chlamydia
The most effective way to avoid getting oral chlamydia is to refrain from engaging in any form of sexual activity. However, it’s understandable that this prevention method may not be ideal or realistic for many people.
The NIH recommends using a barrier method every time you engage in oral sex to reduce your risk for oral chlamydia. Use a condom for oral sex on the penis, and a dental dam for oral sex on the vagina or anus. Another step you can take is to stay in a long-term monogamous relationship with your partner, as having multiple sex partners can often increase your risk for STDs including oral chlamydia.
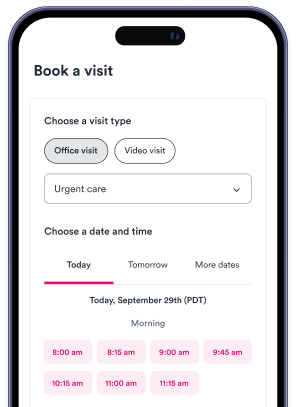
If you’re in need of chlamydia testing, visit Solv today to browse and locate chlamydia testing providers in your area. Solv can help you find a walk-in clinic in your area that offers same-day STD testing, as well as lab testing for other health conditions.
FAQs
What is oral chlamydia?
Oral chlamydia is a sexually transmitted disease that causes symptoms in the mouth and throat.
How is oral chlamydia contracted?
Oral chlamydia can be contracted through oral sex with a partner who is infected with chlamydia.
What are the symptoms of oral chlamydia?
Symptoms may include a sore throat, mouth pain, mouth sores, cold sores, patches of redness with white spots, swollen tonsils, dental problems, and in rare instances, bumps on the tongue.
How is oral chlamydia diagnosed and treated?
Oral chlamydia can be diagnosed with a throat swab test. It can be effectively treated using antibiotics.
What are the risks of untreated chlamydia?
Untreated chlamydia can increase the risk for other serious health problems, including HIV/AIDS, infertility, pelvic inflammatory disease, ectopic pregnancy, infection of the epididymis, and arthritis.