Key points
- Mastitis, an inflammation in the breast, often affects breastfeeding individuals due to clogged ducts or breaks in nipple skin.
- Symptoms include a red, painful, swollen area on the breast, fever, headache, and other flu-like symptoms.
- At-home treatments involve applying cool and warm compresses, wearing a comfortable bra, regular nursing, rest, fluids, and gentle massage.
- Preventive measures include proper latching, changing breastfeeding positions, avoiding tight bras, and breaking baby’s suction around the nipple.
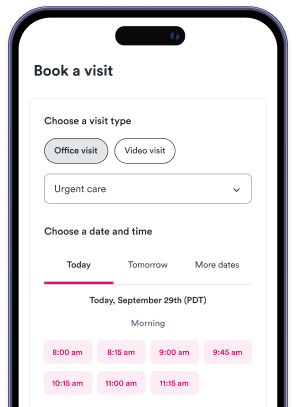
- Urgent care for mastitis should be considered if symptoms worsen or do not improve within 24 to 48 hours. Medical experts may prescribe antibiotics or administer other treatments like therapeutic ultrasound to unclog a milk duct and remedy mastitis.

With so many things to consider in the first few months of a baby’s life, it can sometimes be difficult to prioritize your own needs and well-being. But new moms should be aware that they are more likely to develop certain health conditions that can make activities like breastfeeding a challenge. According to the American Cancer Society, one particular problem called mastitis affects about 20 percent of breastfeeding individuals and can lead to everything from pain and fever to swelling and more. So what is mastitis? Here is everything new moms — and anyone at risk for mastitis — should know.
What is mastitis and what causes it?
Mastitis is inflammation or swelling in the breast that is usually caused by infection. According to the American Cancer Society, the condition can happen due to a variety of causes, but is most common in women who are breastfeeding. The risk of mastitis symptoms is greater during breastfeeding because clogged ducts that prevent milk from properly draining from the breast and/or breaks in the nipple skin can allow infection into the body. When an infection enters the bloodstream, the body’s white blood cells release substances to fight it, which causes increased blood flow and swelling in the area. When this occurs, the infected part of the breast can become painful, red, and warm to the touch. Some people with mastitis also experience fever, headache, or other flu-like symptoms.
“Mastitis most commonly affects women who are breastfeeding but the inflammation can occur for other reasons as well, and can even affect men,” says Solv’s Chief Medical Officer, Rob Rohatsch, MD. “In some cases, non-lactational mastitis can occur in people who have had lumpectomies followed by radiation therapy, those with diabetes, or in people with compromised immune systems. It’s also more likely to affect people who smoke.”
According to the Cleveland Clinic, some other people more likely to develop mastitis are those with:
- Breast implants
- Eczema or other related skin conditions
- Autoimmune diseases
- Nipple piercings
Mastitis symptoms
Mastitis symptoms can vary from person to person, but many people with the condition develop a red, painful, or hot area of swelling on one or both breasts. According to the Cleveland Clinic, this swollen area is often “wedge-shaped” and can feel warm or tender to touch.
“Mastitis rarely affects both breasts, but it can,” Rohatsch says. “It’s perfectly safe to continue breastfeeding with mastitis because the infection — and the antibiotics sometimes used to treat it — can’t be passed through breastmilk. But it’s important to see a doctor if you experience mastitis symptoms so you can receive the right treatment as quickly as possible to avoid further discomfort and other complications.”
In addition to a red, hot, swollen mark on one or both breasts, the signs and symptoms to be aware of, according to the Cleveland Clinic include:
- Pain or burning in the breast that worsens when nursing
- Flu-like symptoms
- Headaches
- Nipple discharge
- Breast lumps
- Fatigue
- Nausea and vomiting
At-home mastitis treatments
“If your symptoms are concerning or getting worse, it’s best to make an appointment with your healthcare provider,” Rohatsch says. “In some cases, they may prescribe an oral antibiotic, which can clear the infection. Mastitis can sometimes go away on its own without medical intervention, but if the infection goes too long without treatment, it can lead to an abscess on the breast. This type of abscess usually needs to be surgically drained, so if mastitis symptoms don’t get better on their own within a few days, see a doctor.”
Try these tips to reduce pain and inflammation as part of your mastitis treatment, according to the Cleveland Clinic:
- Apply cool compresses to your breasts after each breastfeeding session.
- Apply warm, moist compresses or take a warm shower in the hours between breastfeeding sessions.
- Wear a bra that is supportive and comfortable but doesn’t compress the breasts.
- Nurse every two hours or more and avoid going too long between feedings so your breasts don’t overfill with milk (use a breast pump if necessary to express milk between feedings)
- Get as much rest as you can and drink plenty of fluids.
- Take a nonsteroidal anti-inflammatory drug (NSAID) to reduce swelling.
- Gently massage the swollen area of the breast in a circular motion, starting at the outside of the inflamed tissue and working inward toward the nipple.
How to prevent mastitis
Although it’s not always possible to prevent mastitis (particularly in cases where it occurs in non-breastfeeding individuals), those who are breastfeeding can take precautionary measures to minimize the risk of developing the conditions.
“In many cases, working with a lactation consultant may help new mothers develop their breastfeeding technique and avoid complications,” Rohatsch says. “Trained specialists can offer tips and advice so breastfeeding individuals learn the most effective strategies and lower their chances of developing issues like mastitis.”
According to the Mayo Clinic and Cleveland Clinic, a few key techniques can help reduce the risk of mastitis include:
- Allow the baby to completely empty one breast of milk before switching to the other one during breastfeeding sessions.
- Ensure the baby properly latches on during each breastfeeding session.
- Try to change the positioning of your body from one breastfeeding session to the next, which may help empty all areas of the breasts.
- Avoid wearing tight-fitting bras or nursing pads that keep nipples moist and try to air out your nipples after each breastfeeding session.
- If you need to stop a feeding, use your finger to break the baby’s suction around the nipple.
When you should consider urgent care for mastitis
“The longer you wait to treat mastitis, the worse it can get, so it’s important to get medical attention if the symptoms aren’t improving or if they’re getting much worse,” Rohatsch says. “A blocked milk duct will typically improve in 24 to 48 hours, treated or untreated, but if the duct does not seem to be clearing on its own, it’s critical to see a doctor to prevent complications like abscesses from forming.”
Other than prescribing antibiotics, some medical experts may be able to administer other methods of care to unclog a milk duct and remedy mastitis. According to Brigham and Women’s Hospital, therapeutic ultrasound is one potential method for treating blocked milk ducts and mastitis. This type of procedure is usually done by a physical therapist and involves using a device to administer massage and heat to the area, which can help open up the milk ducts and improve circulation to the area. By using sound waves, the ultrasound machine creates vibration in the soft tissues and encourages breast drainage. It’s important to discuss all possible treatment strategies with a medical professional, so seek care immediately if your mastitis symptoms are not well controlled.
Disclaimers
The content provided here and elsewhere on the Solv Health site or mobile app is provided for general informational purposes only. It is not intended as, and Solv Health, Inc. does not provide medical advice, diagnosis, or treatment. Always contact your healthcare provider directly with any questions you may have regarding your health or specific medical advice.
The views expressed by authors and contributors of such content are not endorsed or approved by Solv Health and are intended for informational purposes only. The content is reviewed by Solv Health only to confirm educational value and reader interest. You are encouraged to discuss any questions that you may have about your health with your healthcare provider.
Sources:
- Mastitis (January 25, 2022)
https://www.cancer.org/cancer/breast-cancer/non-cancerous-breast-conditions/mastitis.html#:~:text=Mastitis%20is%20inflammation%20(swelling)%20in,nipple%20can%20lead%20to%20infection
- Breast Infections and Inflammations (2022)
https://www.hopkinsmedicine.org/health/conditions-and-diseases/breast-infections-and-inflammation
- Mastitis (July 22, 2022)
https://www.mayoclinic.org/diseases-conditions/mastitis/symptoms-causes/syc-2037482
- Mastitis (November 10, 2020)
https://my.clevelandclinic.org/health/diseases/15613-mastitis
- Standard of Care: Physical Therapy Treatment of Blocked Milk Ducts (2019)
https://www.brighamandwomens.org/assets/BWH/patients-and-families/rehabilitation-services/pdfs/physical-therapy-treatment-of-blocked-milk-ducts.pdf
FAQs
What is mastitis and who is most likely to get it?
Mastitis is an inflammation or swelling in the breast, typically caused by infection. It's most common in breastfeeding individuals, but can also affect others, including men.
What are the symptoms of mastitis?
Symptoms include a red, painful, swollen area on the breast, fever, headache, and other flu-like symptoms. Some people may also experience nipple discharge or breast lumps.
How can mastitis be treated at home?
At-home treatments include applying cool and warm compresses, wearing a comfortable bra, regular nursing, rest, drinking plenty of fluids, and gently massaging the swollen area.
How can mastitis be prevented?
Preventive measures include ensuring the baby properly latches on during breastfeeding, changing breastfeeding positions, avoiding tight bras, and breaking the baby’s suction around the nipple.
When should I seek medical attention for mastitis?
If symptoms of mastitis aren't improving or are getting worse, it's important to seek medical attention. A blocked milk duct should typically improve in 24 to 48 hours, but if it doesn't, see a doctor to prevent complications.
When should you seek urgent care for mastitis?
You should seek urgent care for mastitis if the symptoms aren’t improving or if they’re getting much worse. A blocked milk duct will typically improve in 24 to 48 hours, treated or untreated, but if the duct does not seem to be clearing on its own, it’s critical to see a doctor to prevent complications like abscesses from forming.
What are some medical treatments for mastitis?
Medical treatments for mastitis can include prescribing antibiotics or administering other methods of care to unclog a milk duct. One potential method for treating blocked milk ducts and mastitis is therapeutic ultrasound, which is usually done by