Key points
- Acid reflux, or GERD, is a digestive condition where stomach acid flows back into the esophagus due to a weakened lower esophageal sphincter (LES), causing symptoms like heartburn and difficulty swallowing.
- Factors such as diet, lifestyle, certain medical conditions, and habits like overeating can influence the functioning of the LES and promote acid reflux episodes.
- Chronic acid reflux can lead to serious complications like esophagitis, Barrett's esophagus, esophageal stricture, and even esophageal cancer if left untreated.
- Treatment for acid reflux includes nonprescription and prescription medications, lifestyle changes, and in severe cases, surgical options like fundoplication and the LINX device.

Acid reflux, or gastroesophageal reflux disease (GERD), is something many people experience. It happens when stomach acid sneaks back up into the esophagus, causing those uncomfortable symptoms we all know too well. This can often occur after enjoying a big, rich meal or if we lie down too quickly after dinner, as gravity isn’t on our side! While it can be annoying to deal with, the American College of Gastroenterology (ACG) explains that acid reflux occurs from time to time. The good news is that it’s usually manageable with some handy home remedies and lifestyle tweaks. In this article, we’ll dive into the symptoms, causes and effective treatment options for acid reflux — aiming to equip you with helpful knowledge to ease any discomfort and keep your digestion running smoothly.
What is acid reflux?
According to the ACG, acid reflux is a digestive condition where there is a backward flow of stomach acid into the esophagus (the tube connecting the throat to the stomach). This occurs when the lower esophageal sphincter (LES), a ring of muscle at the base of the esophagus, becomes weakened or relaxes inappropriately, allowing acid to escape from the stomach. The result can be a range of uncomfortable symptoms, including heartburn, regurgitation and difficulty swallowing.
At its core, acid reflux is a result of a malfunctioning LES, which can be influenced by various factors such as diet, lifestyle and certain medical conditions. Foods that are spicy, fatty or acidic, as well as beverages like coffee and alcohol, can exacerbate the condition. Additionally, habits like overeating, lying down immediately after meals and wearing tight clothing can contribute to increased pressure on the stomach, further promoting acid reflux episodes. While occasional reflux is common and often harmless, chronic acid reflux can lead to more serious complications, including esophagitis, Barrett's esophagus and even esophageal cancer if left untreated.
What are the symptoms of acid reflux?
Individuals experiencing acid reflux may encounter a variety of discomforting signs that can significantly impact their daily lives. Here are some common symptoms associated with acid reflux according to the ACG:
-
Backwash of acid into the throat or mouth (regurgitation)
-
A burning sensation in the chest, commonly known as heartburn
-
Noncardiac chest pain that can mimic heart-related issues
-
Nausea, particularly after meals
-
A sore throat or hoarseness, often due to acid irritation
-
Worsening asthma symptoms or new respiratory issues caused by acid exposure in the airways
What causes acid reflux?
According to the ACG, various factors can contribute to the weakening of the lower esophageal sphincter (LES) or increase pressure on the stomach, leading to the backflow of acid into the esophagus. Here are some of the main causes of acid reflux:
-
Hiatal Hernia: This occurs when a portion of the stomach pushes through the diaphragm into the chest cavity, which can disrupt the normal functioning of the LES and allow acid to escape into the esophagus.
-
Pregnancy: Hormonal changes and increased pressure on the abdomen during pregnancy can lead to relaxation of the LES, making acid reflux more likely, especially in the later stages.
-
Obesity: Excess weight can place additional pressure on the abdomen, pushing stomach contents upward and increasing the risk of acid reflux.
-
Smoking: Smoking can weaken the LES and decrease saliva production (which helps neutralize stomach acid) thereby increasing the likelihood of reflux episodes.
What are the possible complications of chronic acid reflux?
According to the ACG, chronic acid reflux, if left untreated, can lead to a range of serious complications that may significantly affect an individual's health and quality of life. Over time, the repeated exposure of the esophagus to stomach acid can cause damage and various complications. Some potential complications associated with chronic acid reflux include:
-
Esophagitis: Inflammation of the esophagus caused by the corrosive effects of stomach acid, leading to pain, difficulty swallowing and potential bleeding.
-
Barrett’s Esophagus: A condition in which the cells lining the esophagus change due to prolonged acid exposure, increasing the risk of developing esophageal cancer.
-
Esophageal Stricture: Narrowing of the esophagus resulting from scar tissue formation due to chronic inflammation, which can lead to swallowing difficulties.
-
Laryngopharyngeal Reflux (LPR): A condition where stomach acid reaches the throat and voice box, causing symptoms such as hoarseness, chronic cough and throat irritation.
-
Asthma: Acid reflux can exacerbate asthma symptoms or contribute to the development of respiratory issues by irritating the airways.
How is acid reflux diagnosed?
According to the ACG, diagnosing acid reflux typically involves a thorough evaluation by a healthcare professional. If symptoms occur two or more times a week or if over-the-counter medications fail to provide lasting relief, it is essential to consult a doctor to rule out more serious conditions and receive appropriate treatment. To accurately diagnose acid reflux, your doctor may recommend several tests, including:
-
Barium Swallow Radiograph: This imaging test involves swallowing a barium solution that coats the esophagus, allowing X-ray video images to identify abnormalities or reflux.
-
Endoscopy or EGD (Esophagogastroduodenoscopy): A procedure where a flexible tube with a camera is inserted through the throat to visualize the esophagus and stomach, helping to detect inflammation or other issues and allowing biopsies.
-
Esophageal Manometry: This test measures the rhythmic muscle contractions of the esophagus and the function of the lower esophageal sphincter, providing insight into how well the esophagus is working.
-
pH Monitoring: A test that measures the acidity in the esophagus over a 24-hour period, helping to determine the frequency and duration of acid exposure.
What is the medical treatment for acid reflux?
Depending on the severity of the condition and the individual's response to initial therapies, healthcare providers may recommend a combination of nonprescription and prescription medications, as well as surgical options for more persistent cases. Below are the primary treatment alternatives for acid reflux, according to MedlinePlus:
Nonprescription medicines
-
Antacids: These medications neutralize stomach acid, providing quick relief from heartburn and discomfort.
-
Medicines to Reduce Acid Production: H-2 blockers, such as ranitidine and famotidine, decrease the amount of acid produced by the stomach, helping to alleviate symptoms.
-
Medicines that Block Acid Production and Heal the Esophagus: Proton pump inhibitors (PPIs) like omeprazole and esomeprazole not only reduce acid production but also promote healing of the esophagus lining.
Prescription medicines
-
Prescription-strength Proton Pump Inhibitors: Stronger versions of PPIs may be prescribed for individuals with severe acid reflux that does not respond to over-the-counter treatments.
-
Prescription-strength H-2 Blockers: These medications can be more potent than their nonprescription counterparts, providing additional relief for persistent symptoms.
Surgery and other procedures
-
Fundoplication: A surgical procedure that involves wrapping the top of the stomach around the lower esophagus to strengthen the LES and prevent acid reflux.
-
LINX Device: A small ring of magnetic beads is placed around the LES to help keep it closed while allowing food to pass through.
-
Transoral Incisionless Fundoplication (TIF): A minimally invasive procedure that repairs the LES using an endoscope, providing a surgical option without the need for large incisions.
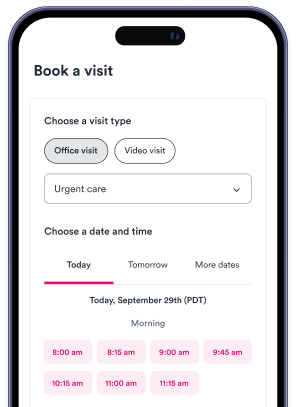
Urgent care near me
If you're experiencing symptoms of acid reflux and need immediate assistance, don't wait any longer. Use Solv to find urgent care near you quickly and easily.
FAQs
What is Acid Reflux or Gastroesophageal Reflux Disease (GERD)?
Acid reflux, also known as Gastroesophageal Reflux Disease (GERD), is a digestive condition where stomach acid flows back into the esophagus. This backward flow occurs when the lower esophageal sphincter (LES), a ring of muscle at the base of the esophagus, weakens or relaxes inappropriately, allowing stomach acid to escape.
What are the common symptoms of Acid Reflux?
The common symptoms of acid reflux include backwash of acid into the throat or mouth, a burning sensation in the chest (heartburn), noncardiac chest pain, nausea after meals, a sore throat or hoarseness, and worsening asthma symptoms or new respiratory issues caused by acid exposure in the airways.
What factors can cause Acid Reflux?
Acid reflux can be caused by various factors such as a hiatal hernia, pregnancy, obesity, and smoking. These factors can contribute to the weakening of the lower esophageal sphincter (LES) or increase pressure on the stomach, leading to the backflow of acid into the esophagus.
Are there any complications associated with chronic Acid Reflux?
Yes, chronic acid reflux, if left untreated, can lead to serious complications such as esophagitis (inflammation of the esophagus), Barrett’s Esophagus (a condition in which the cells lining the esophagus change due to prolonged acid exposure), esophageal stricture (narrowing of the esophagus due to chronic inflammation), Laryngopharyngeal Reflux (LPR), and asthma.
How is Acid Reflux treated?
Acid reflux can be treated with a combination of nonprescription and prescription medications, as well as surgical options for more persistent cases. Nonprescription medicines include antacids, medicines to reduce acid production, and medicines that block acid production and heal the esophagus. Prescription medicines include prescription-strength proton pump inhibitors and H-2 blockers. Surgical options include fundoplication, LINX device, and Transoral Incisionless Fundoplication (TIF).