Key points
- Milia bumps are small, harmless cysts that form when keratin is trapped under the skin, often mistaken for acne or other skin blemishes.
- Milia can be classified into several types, including neonatal, traumatic, multiple eruptive, primary, and secondary, each with different causes and characteristics.
- Factors contributing to milia formation include sun exposure, long-term use of steroids, clogged pores, skin trauma, and certain skin conditions like rosacea or dermatitis.
- Safe removal methods for milia include professional peeling, using retinoids, gentle exfoliation, professional extraction, and avoiding heavy creams; prevention includes sunscreen, moisturizing, regular skin cleansing, and suitable skincare products.

According to the American Academy of Dermatology Association, Milia bumps are small, white cysts that commonly appear on the skin, often around the eyes, cheeks, and nose. These tiny, harmless formations are frequent skin conditions that can affect people of all ages, and while they are not a cause for concern, many seek ways to minimize their appearance. Understanding what milia are and how to safely address them can help individuals feel more confident in their skin. In this article, we will explore the nature of milia, their causes, and effective methods to get rid of them safely, ensuring you can achieve a smoother complexion without compromising your skin's health.
What are milia mumps?
Milia are small, raised bumps that typically appear on the skin's surface, often resembling whiteheads, but are fundamentally different in nature. These tiny cysts are formed when keratin, a protein found in the skin, becomes trapped beneath the outer layer, according to the American Academy of Family Physicians (AAFP). Although milia can occur in anyone, they are most commonly seen in newborns, as well as in adults, particularly around the eyes and cheeks. Understanding the characteristics and causes of milia can help demystify this common skin condition.
Milia are often mistaken for acne or other skin blemishes, but they are actually a type of cyst known as a "keratin cyst." Unlike acne, which is associated with clogged pores and inflammation, milia are not caused by bacteria or oil buildup. Instead, they form when dead skin cells become trapped, leading to the development of these small, painless bumps. While they are harmless and usually resolve on their own, many individuals seek treatment to remove them for cosmetic reasons. Recognizing the benign nature of milia is essential for anyone experiencing this condition, as it reassures them that there is no underlying health risk involved.
Types of milia
Milia can be classified into several types based on their origins and the circumstances under which they develop. Understanding these different types can help individuals identify their specific condition and seek appropriate treatment:
-
Neonatal milia: These small cysts often appear on the faces of newborns and typically resolve on their own within a few weeks.
-
Traumatic milia: These milia develop as a result of skin trauma, such as burns, blisters, or other injuries that disrupt the skin's surface.
-
Multiple eruptive milia: This type occurs when clusters of milia erupt simultaneously, often seen in adults and may be associated with certain skin conditions.
-
Primary milia: These are the most common form of milia and can occur without any underlying skin condition, typically appearing on the face and eyelids.
-
Secondary milia: These develop as a result of skin damage or conditions, such as prolonged sun exposure or the use of heavy creams that block pores.
What causes milia?
While the exact reasons for their formation can vary, several common factors contribute to the development of these small cysts. Here are some of the primary causes of milia according to the AAFP:
-
Sun exposure: Prolonged exposure to ultraviolet (UV) rays can damage the skin and lead to the formation of milia, particularly in sun-sensitive areas.
-
Long-term use of steroids: Topical or systemic steroids can thin the skin and disrupt the natural shedding of dead skin cells, increasing the likelihood of milia.
-
Clogged pores: When dead skin cells accumulate and block the pores, they can trap keratin beneath the surface, resulting in the formation of milia.
-
Skin trauma: Injuries such as burns, blisters, or other skin damage can lead to the development of traumatic milia in the affected areas.
-
Certain skin conditions: Conditions like rosacea or dermatitis can also contribute to milia formation by affecting the skin's natural exfoliation process.
Milia removal
When removing milia, it's important to approach the process safely to avoid irritation or damage to the skin. Various methods can effectively reduce or eliminate milia, allowing individuals to achieve a smoother complexion. According to the AAFP, here are some safe and recommended treatments to discuss with your pediatrician:
-
Peeling the area: Professional chemical peels can help exfoliate the skin and promote the shedding of dead skin cells, which may reduce the appearance of milia.
-
Using retinoids: Topical retinoids can enhance cell turnover and prevent the buildup of keratin, making them an effective treatment for milia over time.
-
Gentle exfoliation: Incorporating gentle exfoliating products, such as alpha-hydroxy acids (AHAs) or beta-hydroxy acids (BHAs), can help remove dead skin cells and reduce milia formation.
-
Professional extraction: Consulting a dermatologist for professional extraction can safely remove stubborn milia using sterile tools and techniques.
-
Avoiding heavy creams: Switching to lighter, non-comedogenic skincare products can help prevent clogged pores, reducing the likelihood of milia developing in the first place.
How to identify and prevent milia
Recognizing the signs of milia—such as small, white, painless bumps on the skin—can prompt timely action to address them. Additionally, adopting a proactive skincare routine can significantly reduce the risk of developing milia in the first place. Here are some effective ways to prevent milia according to the AAFP:
-
Use sunscreen: Protecting your skin from harmful UV rays can prevent sun damage, which is a contributing factor to milia formation.
-
Moisturize: Keeping your skin well-hydrated with non-comedogenic moisturizers helps maintain a healthy skin barrier and promotes proper exfoliation.
-
Clean your skin frequently: Regularly cleansing your face helps remove dirt, oil, and dead skin cells, reducing the chances of clogged pores that lead to milia.
-
Exfoliate regularly: Incorporating gentle exfoliation into your skincare routine can help eliminate dead skin cells and promote cell turnover, preventing milia buildup.
-
Choose suitable skincare products: Opting for lightweight, non-comedogenic products can help minimize the risk of clogged pores and the subsequent formation of milia.
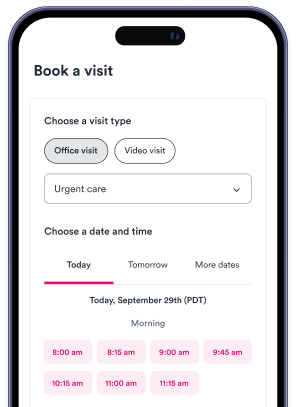
Urgent care near me
If you're dealing with skin concerns like milia or any other urgent health issue, don't hesitate to seek professional help. Solv makes it easy to find urgent care facilities near you, ensuring you receive the attention you need quickly and conveniently.
FAQs
What are milia bumps and what causes them?
Milia bumps are small, white cysts that commonly appear on the skin, often around the eyes, cheeks, and nose. They are formed when keratin, a protein found in the skin, becomes trapped beneath the outer layer. They are not caused by bacteria or oil buildup, but rather when dead skin cells become trapped. Certain factors such as sun exposure, long-term use of steroids, clogged pores, skin trauma, and certain skin conditions can contribute to their formation.
Are milia bumps harmful or a cause for concern?
No, milia bumps are harmless and usually resolve on their own. They are not a sign of any underlying health risk. However, many individuals seek treatment to remove them for cosmetic reasons.
What are the different types of milia?
Milia can be classified into several types including neonatal milia, which appear on the faces of newborns; traumatic milia, which develop as a result of skin trauma; multiple eruptive milia, which occur when clusters of milia erupt simultaneously; primary milia, the most common form that can occur without any underlying skin condition; and secondary milia, which develop as a result of skin damage or conditions.
How can milia be safely removed?
Safe methods for milia removal include professional chemical peels, using topical retinoids, gentle exfoliation, professional extraction by a dermatologist, and avoiding heavy creams. These methods can help reduce or eliminate milia without damaging the skin.
How can the formation of milia be prevented?
Preventative measures include using sunscreen to protect from harmful UV rays, moisturizing with non-comedogenic products, regularly cleansing the face, incorporating gentle exfoliation into your skincare routine, and choosing suitable lightweight skincare products. These steps can help maintain a healthy skin barrier, promote proper exfoliation, and prevent clogged pores.